We Deserve More: Rethinking Mental Healthcare for Real Healing
The mental healthcare system isn’t just failing—it was never designed to truly support us. From involuntary hospitalizations to impersonal, overburdened care, too many people seeking help are met with control instead of compassion. In this piece, I share my own experience of being denied autonomy and dignity in the system, and why we must rethink mental healthcare to center real healing. We deserve more—and it’s time to demand it.
Cam Abbott
2/22/20254 min read
Current State of the Mental Healthcare System:
Insufficient funding leaves providers underpaid and patients underserved.
A nationwide shortage of mental health professionals—especially in rural communities—makes timely care nearly impossible.
Insurance barriers prevent people from accessing the help they need.
Stigma and bureaucratic red tape push them even further from support.
The system is fragmented, under-resourced, and inaccessible to many.
But here’s the difficult truth... the system isn’t broken by accident:
It is outdated, overburdened and structured in ways that don’t always prioritize the well-being of the people it’s meant to serve.
It leans on short-term fixes—medication over therapy, crisis intervention over prevention—because those are the profitable options it was built to pursue.
The Mental Healthcare System Is Failing Us—
It’s Time to Rebuild
Meanwhile, community-driven, patient-centered solutions remain underfunded and overlooked.
The result? Millions of people unable to get the care they need, when they need it.
I didn’t call the right person.
I didn’t explain my situation well enough.
I should’ve asked what the medication was for.
One of my most traumatic experiences in involuntary care happened over my 25th birthday. I had been hospitalized before, and I thought I knew what to expect—how to “play by the rules” to ensure a safe and manageable stay. But I quickly realized that no amount of experience could prepare me for what was ahead.
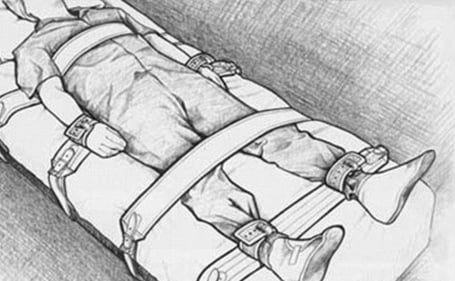
After being forcibly restrained and medicated—I woke up in a hospital bed to a set of papers stating that I would receive medical treatment against my will. The paper was given to me a full week after I had submitted a formal request for a 72-hour release, a legal right that is rarely upheld. Many of us in the hospital couldn’t understand why this request existed at all if it was never respected. Soon after, I was informed that I would have to go to court—not only against my doctor but eventually against my own family—to fight for my release.
My story is not unique.
It highlights what so many others have endured:
Impersonal, overburdened treatment
Lack of trauma-informed care
Complete disregard for patient autonomy
I was lucky to make it out. But no one should have to feel “lucky” to survive the mental healthcare system.
When seeking mental healthcare, we are often at our most vulnerable. We may lack the resources, support, or even the personal agency to advocate for ourselves. And yet, nothing truly prepares you for the reality of navigating a system that seems designed to work against you rather than for you.
I have experienced nearly every level of care—voluntary and involuntary hospitalization, inpatient and outpatient programs, and intensive partial hospitalization. Each time, I have walked away believing that I should have done something differently.

This Isn’t About Blame—It’s About Change
Meanwhile, patients are stripped of their autonomy and left to navigate a system that prioritizes compliance over genuine support.
Stripped of Autonomy:
What Happened When I Needed Help
How the System Took My Autonomy
How We Rebuild: A Vision for Mental Healthcare That Actually Works
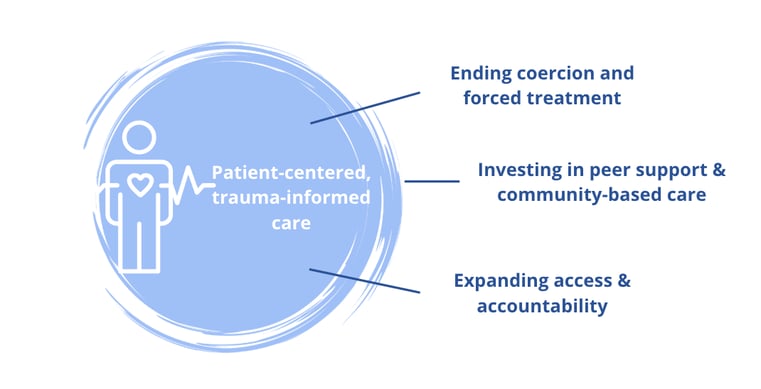
If we want to build a system that supports patients rather than harms them, we must fundamentally reimagine how care is delivered.
Today’s healthcare is too often driven by profitability and compliance, sidelining the patient’s true needs. Instead, we need a model that centers on the individual, incorporates trauma-informed practices, and invests in peer support and community-based care.
As highlighted by NAMI, “people receiving peer-support services were less likely to end up in hospitals and more likely to engage with their treatment providers.” By embracing peer support, grounded in shared experiences and mutual empowerment, we foster a sense of community that fosters healing and encourages individuals to proactively seek care before a crisis occurs.
We Deserve More—And It’s Time to Demand It
This Won’t Change on Its Own—We Have to Push for Reform


Survival isn’t enough. If we want a mental healthcare system that actually serves us, we have to rethink it, rebuild it, and refuse to settle for anything less.
But the truth is, these mistakes should never fall on the patient.
Advocating for yourself—especially in a moment of crisis—should not be an individual burden.
And yet, within our current system, it is.
The reality of mental healthcare in the U.S. is that professionals and institutions are:
Overburdened
Understaffed
Not properly trained in trauma-informed care
If we want better outcomes, we need a better system—one that actually supports people, rather than trapping them in cycles of fear and powerlessness.
This piece will cover:
The structural issues that make quality care so difficult to access
How these barriers play out in practice, including my own experience
A vision for rebuilding mental healthcare into something that actually serve people, not controls them